The New "How to Avoid COVID"
UPDATED: April 29, 2024
COVID Prevention
An effective multilayered approach to COVID prevention should include proven measures such as masking with high-quality respirators (N95s, KN96s, KF94s or better), improving indoor air quality with ventilation and filtration, physical distancing, getting the latest vaccines, and using COVID tests appropriately. Unproven methods should not be considered part of a multilayered approach. Topical nasal products such as sprays or ointments may seem tempting but are not proven to prevent COVID infections (none are FDA approved for COVID) and may have risks. For example, Vaseline and petrolatum-based ointments can cause pneumonia if applied to the inside of the nose, as they may be subsequently inhaled where they can damage the lungs. Over-the-counter antibiotic ointments are intended to protect from bacterial infection in minor skin wounds and should not be used inside the nose. Although early research on other uses has been publicized, given the risks of petrolatum-based ointments if used in the nose, it is important to wait for larger scale studies to understand both potential risks and benefits. Colloidal silver, sometimes touted in nasal spray form, is not proven to treat or prevent any medical condition and can cause permanent gray pigmentation of the skin as well as other serious side effects. Research studies shared in the news or on social media should not be used in place of medical advice from an individual healthcare provider you trust.—People's CDC <peoplescdc@substack.com> April 29, 2024
This information is addressed primarily to tenants of public or subsidized housing for elderly and disabled persons. COVID is an airborne infectious disease spread by the air we share with others. The best way to control disease and protect people from infection is to use public health measures, rather than only to depend on small groups or individuals to protect themselves. I present ideas that an individual or a housing community to use to reduce the chance of infection.
What can a person do amidst a pandemic? I address this challenge.We as a society seem unable to accept some discomfort, such as enforced mandates on vaccination requirements, masking, and indoor gatherings and then are surprised when large numbers of people sicken and die, key supports to our lives crash, and we are forced into a severe lockdown to survive. We should be relating to the leading indicators, not the full hospitals or the death rates. That is basic public health. We need a public health response from every level of government.
The President, the Governor, my landlord, and our society have not learned from our experience with COVID in 2020 and 2021.
First step, see what is happening in the environment, then take steps appropriate to your risk tolerance and vulnerability.
New variants pose renewed threat because they can evade the body's defenses, even despite vaccination and boosting. Be very careful.
How long can you be infectious?
When the US Centers for Disease Control and Prevention (CDC) halved its recommended isolation time for people with COVID-19 to five days back in December, it said that the change was motivated by science. Specifically, the CDC said that most SARS-CoV-2 transmission occurs early in the course of the illness, in the one to two days before the onset of symptoms and for two to three days after.
Many scientists disputed that decision then and they continue to do so. Such dissent is bolstered by a series of studies confirming that many people with COVID-19 remain infectious well into the second week after they first experience symptoms. Reductions in the length of the recommended isolation period — now common around the world — are driven by politics, they say, rather than any reassuring new data.
“The facts of how long people are infectious for have not really changed,” says Amy Barczak, an infectious-disease specialist at Massachusetts General Hospital in Boston. “There is not data to support five days or anything shorter than ten days [of isolation].” Barczak’s own research, published on the medRxiv preprint server, suggests that one-quarter of people who have caught the Omicron variant of SARS-CoV-2 could still be infectious after eight days.—Nature News, July 26, 2022
Leading Indicators of COVID in the Community
COVID-19 Dashboard
Massachusetts Department of Public Health, COVID-19 Dashboard, Weekly Data by City and Town This is the source for positivity data cited in this paper.
Wastewater COVID-19 Tracking by Massachusetts Water Resources Authority
Evidence of COVID in wastewater samples has emerged as a leading indicator of COVID infections likely to appear in ~10 days.
Test results from MWRA’s pilot study to track wastewater at the Deer Island Treatment Plant for indicators of COVID-19 infection are posted on this site.
Samples are currently taken 3 - 7 times a week and analyzed by Biobot Analytics, a wastewater epidemiology company. Data are updated as received by Biobot following an internal review process.
For some county wastewater data from go to Biobotic Analytics
Current transmission information for Essex County and Peabody, Massachusetts
Will the new CDC guidelines protect us?
No, they are designed to protect hospitals from being overwhelmed by severe COVID cases. We need to focus on our immediate local community and the places where we live. We can do this by paying attention to the rate of disease transmission and by working together.
The current CDC guidelines are designed to protect hospitals from too many people with severe disease. This approach ignores the so-called less severe cases, "mild disease," that can nevertheless create long COVID with continuing, disabling, chronic harm. And the CDC guidelines leave those at greatest risk unprotected by community actions, including children too young to be vaccinated, those with compromised immune systems, elderly, disabled, and those with various conditions making them more susceptible. Therefore, it is imperative that such vulnerable populations take all possible steps to protect against infection and to mitigate disease.
Nursing homes, assisted living homes, and housing for the elderly and disabled are all high-risk environments.
Even people who have had "mild" COVID and have not been hospitalized can experience serious, continuing health problems. Clearly, avoiding infection remains important.
In summary, using a national cohort of people with COVID-19, we show that risk and 12-month burden of incident cardiovascular disease are substantial and span several cardiovascular disease categories (ischemic and non-ischemic heart disease, dysrhythmias and others). The risks and burdens of cardiovascular disease were evident even among those whose acute COVID-19 did not necessitate hospitalization. Care pathways of people who survived the acute episode of COVID-19 should include attention to cardiovascular health and disease.--- Xie, Y., Xu, E., Bowe, B. et al. Long-term cardiovascular outcomes of COVID-19. Nat Med (2022).
"We have met the enemy and he is us."
Denial and complacency, that's how our leaders and many of us are thinking about COVID. Off with the masks! Let's eat, sing, and dance, all together! COVID is gone, we're all safe now.
Really? People are still getting sick and dying. Many are experiencing "long covid," debilitated by symptoms that puzzle doctors.
Worst of all, by forgetting the past and ignoring the threat of future infections, we are doomed to another terrible round of disaster.
We know what to do, and the President has a plan. But the Congress hasn't allocated the money. What needs to happen: we need to watch for a new wave, watch for a new version of COVID or some other new disease, we need to have high-quality masks on hand, new medicines available, test kits available, keep pushing for everyone to vaccinate and boost, and more. We have seen how infections in China and Europe quickly arrive here. Today, there is a surge of illness with a new version of COVID. We need to be ready because it will surely come here soon. Here's the stark warning by Eric Topol:
Now is the wrong time to become complacent. Our vaccination and booster rates have left us in a highly vulnerable position, worse than many low and middle-income countries. Premature cessation of mitigation measures, particularly in many regions of the country with high levels of circulating virus, leaves our immunocompromised population susceptible. The math for a more harmful version of the virus is unfavorable. Unwillingness to support a solid plan to be prepared—for the first time in the American pandemic—is looming. The United States has performed poorly relative to peer countries from the start of the pandemic. Not taking advantage of this moment to get ahead of the virus, instead of being entranced with a false sense of security, will just add to a historic big miss.---Eric Topol, The Epidemic of Covid Complacency, Ground Truths, March 6, 2022.
Who will save us?
Charity Dean MD, MPH&TM was Assistant Director for the California Department of Public Health and was a key member of the executive team directing the COVID-19 outbreak response. A brilliant and dedicated physician and public health leader, Dean concluded that our public health system is not adequate. She said,
‘Stop waiting for someone to come and save you. Because no one is coming to save you.’---Lewis, Michael. The Premonition: A Pandemic Story (p. 42). W. W. Norton & Company. Kindle Edition.
I have been frustrated by the failure of our national and state public health responses, and see that our local health department, which has been responsive, is constrained by the policies of state and regional public health departments, by citizens who don't want mandated restrictions, and by a lack of resources.
Coronavirus Crisis Update: Interview of Charity Dean. She narrates her personal experiences as a public health officer battling COVID and her decision to create a company to create a way to track and prevent disease spread, and to integrate health and public health systems.
So, perhaps we can follow the lead of Charity Dean and adapt her idea for local responsibility. She proposed that each local community would have to use local data to determine what actions they would take, what level of risk they were willing to tolerate. If people took these decisions into their own hands, they could stop blaming the government.
It wasn’t just the effects of the virus that needed to be mitigated. The effects of the culture did, too. For the plan to work, Charity thought, it needed to be locally controlled. Each zip code would be able to see what it needed to do if it wanted to relax restrictions. And each zip code would have its own leaders, who would know the best ways to encourage good behavior. The one shot America had at behaving well, and thus saving itself, was to remove the feeling that “the government” was imposing restrictions on people and re-instill the idea that people were imposing order on themselves, to fight a common enemy.---Lewis, Michael. The Premonition: A Pandemic Story (p. 236). W. W. Norton & Company. Kindle Edition."
Unfortunately, in my opinion, our country has divided along political and belief systems so that it is hard to see how a purely democratic approach to public health can succeed.
But in residential situations where the landlord and management take leadership roles and work with tenants, all are protected from COVID and all---staff as well as tenants---have a more positive experience as a community.
We will have to save ourselves
Nevertheless, we can try to develop practical solutions based on collaboration between landlord and tenants.
We should use the two-week positivity rate as reported on the COVID-19 Dashboard, Massachusetts Department of Public Health, because it is a good indicator of current community transmission and incidence. Masking is one key element of a protective system, there are many additional elements.
Here is the solution that I am proposing to my landlord.
-
When the two-week positivity rate of either Essex County or City of Peabody rate is below 1%, protective masking is not required; take down the signs requiring masking; masking is optional, encourage for people with symptoms or exposure or special vulnerability.
-
When the two-week positivity rate of either Essex or Peabody is 1.5% or higher, commence protective masking and post signs.
-
Improved management policies
CDC: National Wastewater Surveillance System (NWSS)
Wastewater surveillance can provide an early warning of COVID-19’s spread in communities. People infected with SARS-CoV-2 can shed the virus in their feces, even if they don’t have symptoms. The virus can then be detected in wastewater, enabling wastewater surveillance to capture presence of SARS-CoV-2 shed by people with and without symptoms. This allows wastewater surveillance to serve as an early warning that COVID-19 is spreading in a community. Once health departments are aware, communities can act quickly to prevent the spread of COVID-19. Data from wastewater testing support public health mitigation strategies by providing additional crucial information about the prevalence of COVID-19 in a community.
How can I keep safe from COVID?
- Vaccination
- booster
- masking with N95, KN95, or KF95 respirator.
- avoid indoor gatherings, limit time of exposure
- ventilation & filter air
- clean hands
- to keep others safe and know my status, rapid tests
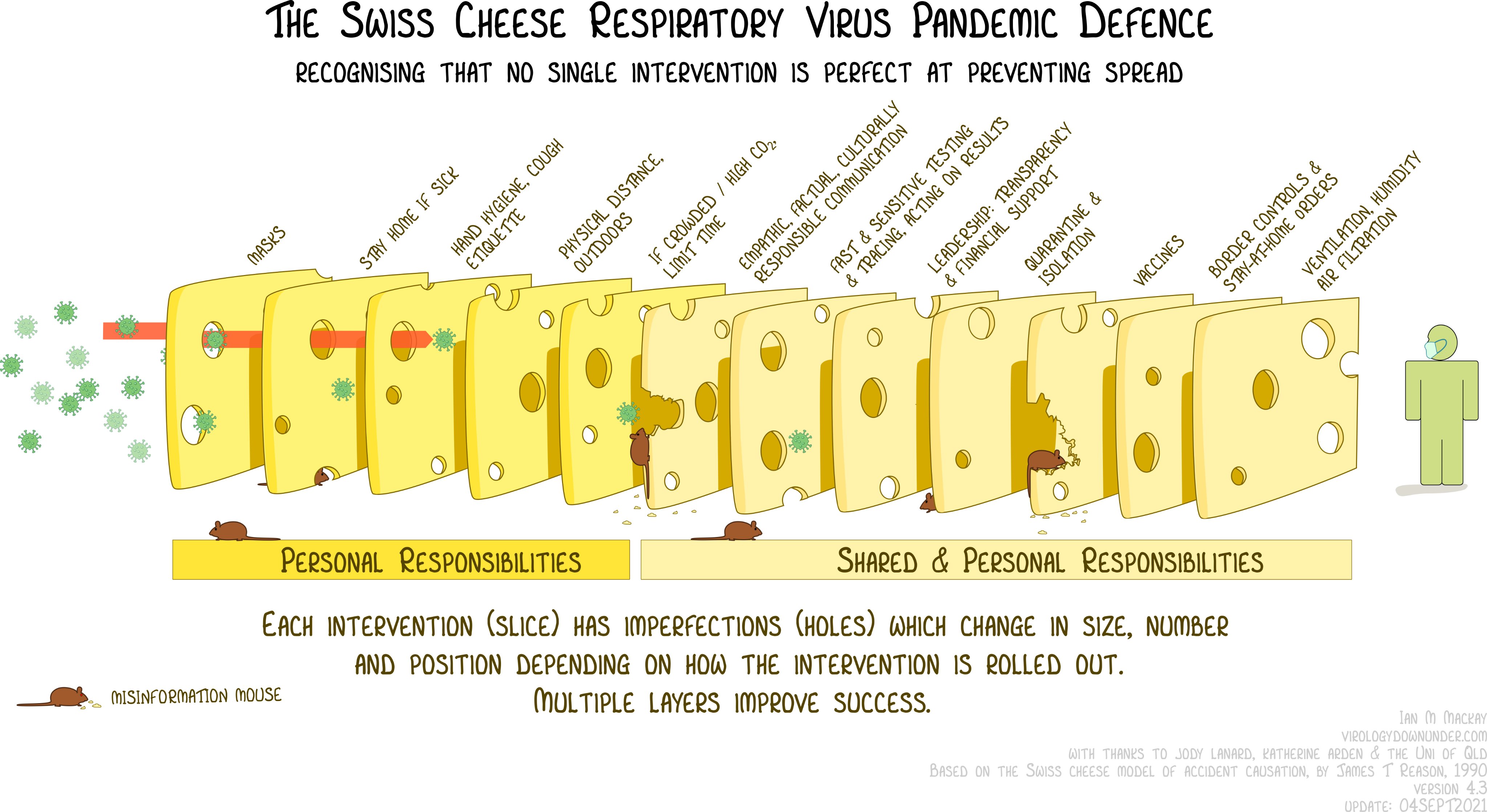
The Swiss Cheese Method
Residential community issues
What can a residential community do for mutual protection? A landlord and management can take many steps, ideally in concert with tenants. Earlier reports demonstrate that tenants can enjoy significantly increased safety if everyone works on behalf of the community. A zero-tolerance policy to require and enforce masking by everyone in public areas of the residential setting is important. N95 masks should be available to everyone. Vaccination and boosting is essential for individual as well as community protection. At times, restricting access to common areas may be needed. Because testing has many practical limitations, one should assume that everyone in a room is infectious, regardless of their vaccination or test status. For example, omicron ramps up so quickly that a negative test may only be valid for a few hours.
Landlord has significant responsibility
I have had COVID and was in hospital for 6 days, and almost a year later, have not fully recovered my stamina. Although I have had two vaccinations and a booster, I am in a vulnerable category (age, asthma & other lung health issues) and therefore highly motivated to avoid another experience of COVID.
For two months I have been seeking to have my landlord provide an accommodation to protect me, as a person with a disability, from exposure to COVID. I asked them to enforce their own rule for universal masking in the public areas of the apartment building.
My landlord has recognized my right to an accommodation for protection, however they have done nothing effective, such as actively enforcing masking. There are 88 apartment units for elderly and elderly disabled persons, all of whom are at an elevated risk from COVID.
When I sought the accommodation, the 14-day positivity rate was already alarming at 2.5%. The 14-day Percent Positivity had declined to 2.15% on March 3,
Months later, my landlord has not implemented an effective accommodation.
The failure of my landlord to implement their own policy and their legal obligation to provide an accommodation to enable a person with a disability to enjoy their residence in safety puts me at risk. Implementing an effective and enforced policy on masking would protect everyone in the building.
This is "deja vu" all over again. The President, the Governor, my landlord, and our society have not learned from our experience with COVID in 2020 and 2021. Testimony to Joint Committee on Covid-19
Tenant responsibility
Even where a landlord is responsive and compassionate, it is difficult to create a tenants association that can advocate for the needs and rights of tenants and mobilize tenants for their common good.
It is difficult and perilous to try to organize tenants when the landlord is indifferent or hostile.
Where I live, we did have a good tenants association that was able to secure our rights and provide a warm social environment. However, bullying and mobbing brought that effort to an end, hastened by the active hostility of management. Thus, when we have faced the COVID crisis in the past again today, our ability to organize for the common good was already weak. The threat of renewed bullying and harassment, plus the inability to hold meetings posed barriers. And the landlord has not even shown that they will enforce their own rules and regulations, such as masking. This is a statewide and even a national context for tenants in public and subsidized housing.
This is not evasion of responsibility, but an honest appraisal of the problem. We know that, where the landlord takes a positive stand, tenants can and do take responsibility for each other.
The danger around us
Hospitals are struggling to manage the continuing influx of cases of COVID and other medical conditions. The health system is close to collapse.
The older you are, the more likely we are to have more severe illness, and much worse if we are not vaccinated. Over 80 years, we are more likely to die, and if not vaccinated, much more at risk.
Mild COVID will likely make the patient miserable and can result in long COVID, with long term health problems. JD Davids, who works with networks of disabled and chronically ill people, reports that,
“...it’s been abundantly clear for more than a year that even asymptomatic infection brings a significant risk of long Covid – a wide spectrum of more than 200 symptoms and conditions that can appear months after initial infection or apparent recovery, and leave children, adults and elders disabled, chronically ill and desperate for medical care, income, housing or even recognition that their suffering is from real physical conditions. “
How can we stay safe and avoid infection?
The news about COVID has been alarming and the advice has been confusing. Here is my understanding of how I can stay safe. Remember, I can’t give medical advice. But I can read what experts are saying and select the soundest conclusions to share with you.
- Vaccination
- booster
- masking with N95, KN95, or KF95 respirator.
- clean hands
- avoid indoor gatherings
- ventilation & air filter
- rapid tests to know your status & protect others
COVID IS AIRBORNE!
COVID spreads from an infectious individual through every breath they exhale, full droplets and tiny virus particles in an invisible cloud, or aerosol. It took a long time for the public health and medical communities to recognize this fact, leading to the failure to prescribe the most effective techniques for mitigating the epidemic.
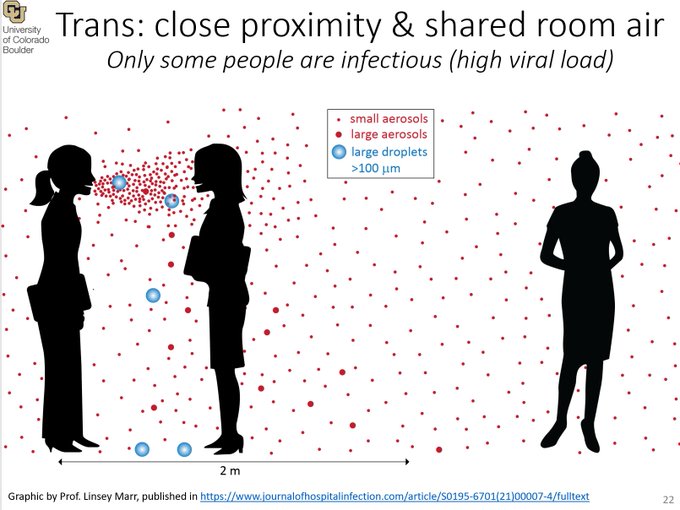
People who are close are exposed to droplets from each other; everyone in a room is exposed to aerosols from all others. One infected person can spread infection to all others in the room.
The key to staying safe and avoiding infection, or if I am infected, for protecting others, is to avoid breathing the COVID aerosol in the air from another person.
Warning: SARS-2 is airborne. Watch those poorly ventilated indoor corridors which can fill with air from surrounding rooms. Even if you don't see anyone else, wear a mask at all times indoors.--https://twitter.com/kprather88
How can I keep from breathing infected air?
-
Evaluate the risk and danger in every situation.
-
Ventilation from open windows, fans, filters can dilute the aerosols.
-
Distance from others: 6 feet is not enough; anyplace in a room where there is even one infected person is risky. The more people in the room, the higher the chance that someone is infectious; we have no fully reliable test system that can guide us in our daily lives.
-
Outside is safer than indoors.
-
Indoors, fewer people is safer than a crowd mainly because there is an increased chance of there being an infectious person, and because more people are exposed to potential infection.
-
Indoors, good quality masks, fitted to have no leaks, worn by everyone.
-
Avoid spending time indoors with others, less time is safer.
-
The more forcefully people breathe, as in shouting, singing, or during heavy exercise, the more aerosols will be present.
-
The more ventilation and filtration there is, the aerosols will be diluted.
-
Continue hand washing, sanitizer.
-
Rapid tests by everyone helps to prevent spread

Steps for safety
There are several steps I can take to say safe. No one step is 100% able to protect, but by using the idea of several actions like layers of swiss cheese slices so that the holes don’t line up, I can improve my chances.
The first step is to know how much COVID is in my area or my apartment building so I can know my risk for shopping, or hanging out with neighbors. I can use an online risk calculator, the one I like tells me that a one-hour shopping trip is highly dangerous. I can input several key factors about a context, say, to go shopping for food, what kinds of masks are people wearing, how far apart are they from me, and more; and get guidance on the level of risk. The results are influenced by the reported level of disease in the community.
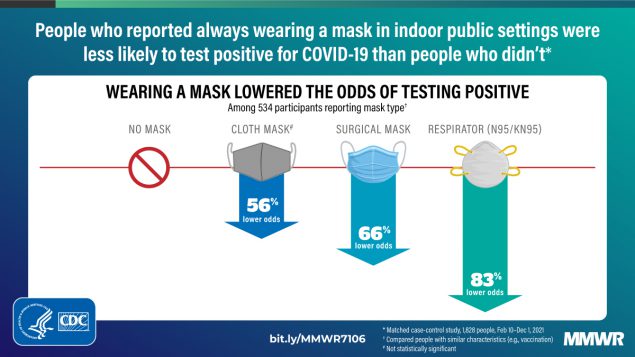
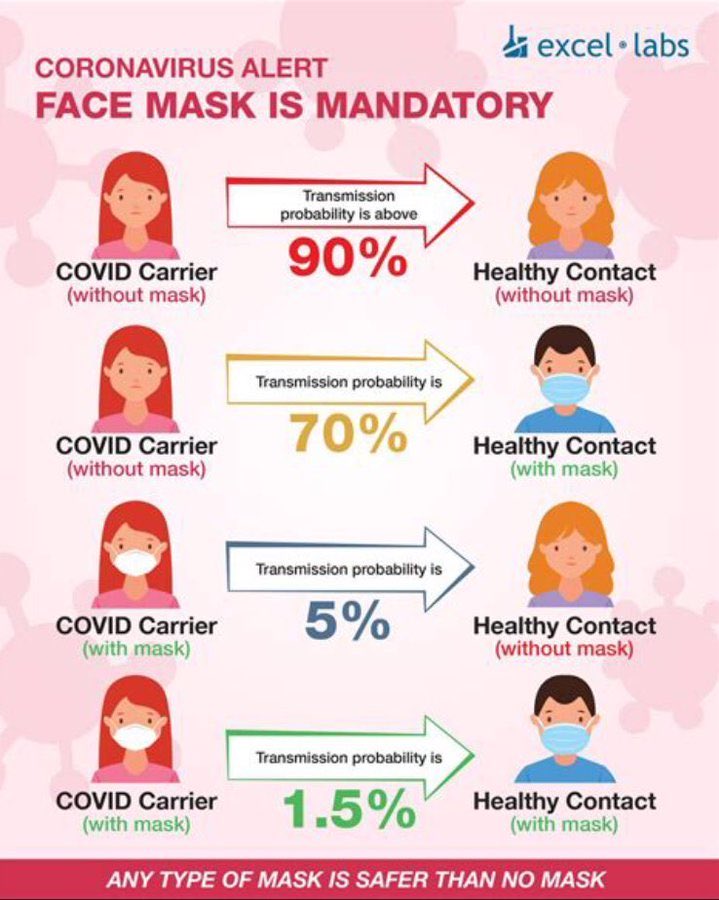
Masking protects against infection. N95, KN95, or KF95 respirators offer the best protection.
In addition to being up to date with recommended COVID-19 vaccinations, consistently wearing a comfortable, well-fitting face mask or respirator in indoor public settings protects against acquisition of SARS-CoV-2 infection; a respirator offers the best protection. Andrejko KL, Pry JM, Myers JF, et al. Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California, February–December 2021. MMWR Morb Mortal Wkly Rep 2022;71:212–216. DOI: http://dx.doi.org/10.15585/mmwr.mm7106e1external icon.
Leading indicators
I like to use what are called leading indicators, some source of information that tells me the expected level of infections, cases, hospitalizations, and deaths that will follow.
Waste-water testing serves as an early warning sign for a COVID-19 surge. Cambridge-based Biobot Analytics, which tests the waste water coming into MWRA’s Deer Island treatment plant, has said it has found the amount of virus in the waste water is correlated with newly diagnosed coronavirus cases four to 10 days later. The amount of virus in wastewater has jumped to very high levels.
The two-week positivity rate is an excellent leading indicator. Over the last couple of months the 2-week positivity rate in Peabody, where I live, has risen rapidly, from 2.5% to 21.74%. People have traveled and mingled for Thanksgiving, Christmas, and New Year. And the leading indicators continue to rise even while the medical system is on the verge of collapse.
Action steps
Official governmental actions
I have been unable to understand the reluctance of officials to mandate masking and/or restrictions on gatherings as a way to slow the increase of infections. Such mandates are indeed unpopular. Many people argue for the need to keep normal commercial and social activity, "Kids belong in school," and some reject mandates for the common good as infringement on their individual "rights." Restrictions on gyms, restaurants, religious worship gatherings, and other indoor events deprive people of normal activity and put employees out of work.
Such failure to act seems based on the costs of action, but absent consideration of the costs of failure to act.
However, when such mitigation measures are applied early in the course of an epidemic, they can prevent much illness, suffering, death, and long-term chronic disease. Absent the leadership to act early, society may be crippled by the effects of the collapse of the medical system, the lack of essential workers sidelined by illness or death, and the breakdown of the complex chains of goods and services which sustain social life. A breakdown of civil order could follow.
In housing
In housing for the elderly and disabled, some management regimes strive to protect tenants and staff from harm. In others there is indifference and incompetence.
The elements for success may include:
- Landlord/management acts early and firmly to prevent the spread of infection. Gatherings may be restricted, masks required.
- Landlord/management has a zero-tolerance policy for masking and other mandates.
- N95 masks and rapid tests should be available to all for free or very low cost. N95 means that the mask will block 95% of aerosols that carry COVID.
- Management works with tenants to enable voluntary reporting and to provide essential support for people who must be in seclusion. Tenants work together and with management to establish and maintain a climate of respect and caring. Services and social connection (phone, email, zoom) provided to support people in seclusion.
- Some examples at: Testimony to Joint Committee on Covid-19
Rapid at home tests use antigens to detect levels of virus that may make a person infectious. The tests, sometimes called “lateral flow tests,” are not perfect. And they need to be used frequently, even daily, because omicron spreads quickly and the virus can replicate in the body very quickly. And sometimes the tests don’t catch an infectious person. Nevertheless, if you can obtain at home antigen tests, they offer guidance. Am I infected? Am I still infectious, or must I stay in quarantine or isolation?
Michael Mina, a physician and epidemiologist has long advocated the use of rapid antigen tests as an aid to surveillance, that is, watching for disease. He writes on Twitter in response to criticisms of rapid tests that don’t always provide valid results, that
“Rapid tests DO work. Nothing in public health is perfect, not vaccines, masks, quarantines. Rapid tests are the single most accurate indicator of whether you are infectious and whether you are a risk to others (that the average person not in a research lab can have access to).”
Mina on twitter argues that rapid tests do the job of telling you when you are infectious.
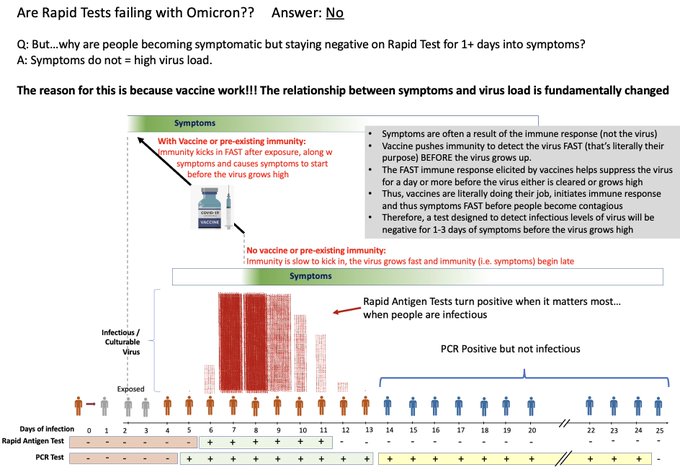
To see if am currently infectious, I can use a series of rapid antigen testing every day.
Here is the British NHS video for their kits. It has a good demonstration of the right way to wash your hands. There is a lot of information you can skip, it talks about collecting for a kit to be sent to a lab. Just pay attention to the swab procedure and use the at-home kit.
Rapid antigen tests show positive when I have a level of virus high enough to make me infectious to others. The virus can grow rapidly and cause me to be infectious only hours after I tested negative.
Throat swabs?
We are seeing new reports that omicron can be found in the throat and in saliva earlier and more reliably than in the nose. Some reports say that antigen tests are more reliable if one first swabs the throat, then both nostrils. People are reporting that a nasal swab comes up as negative for COVID, and that a throat plus nasal swab then shows positive for COVID. The FDA advises against untrained persons doing throat swabs. The validity of using the current rapid tests with throat swabs has not been evaluated.
Here’s my own recipe
I have had COVID; I am vaccinated; I got a booster.
I wear a mask indoors except in my own apartment. When I leave my apartment I am always masked unless I am outdoors and distant from others. I use N95; also good are KN95, or KF95. Surgical masks may be effective if there are no leaks, as by wearing a retainer (“mask sealer, mask brace”) over the mask.
Rotate masks
I use one N95 mask for each day of the week and put it aside for a week after use, the virus won’t live that long. I discard the masks and use a new set if they get wet, dirty, or have been in use for several weeks. One source suggests that a total of 40 hours use in a rotation is OK. This article gives some guidelines. Thus, at $1.00/mask, 7-10 masks costs $10, and can protect me for several weeks, because I need to wear a mask for short times. A non-profit, Project 95, stocks a variety of masks at good prices. I am using a duckbill type mask that is relatively easy to breathe through, and they are available for $0.74 each in a box of 50 plus shipping. Armbrust is a reliable commercial company that I have used; they make surgical masks in Texas and market masks and respirators made by other companies. A comparative chart of several types of masks confirms value of highest-level mask without leaks.
A surgical mask system can be as effective as an N95 respirator at preventing the spread of virus (source control), according to recent tests of surgical masks reported in the American Journal of Infection Control. Read "≥42%" as "at least 42%" because the symbol stands for "equal or greater than."
“Medical masks without modification blocked ≥56% of cough aerosols and ≥42% of exhaled aerosols. Modifying fit by crossing the earloops or placing a bracket under the mask did not increase performance, while using earloop toggles, an earloop strap, and knotting and tucking the mask increased performance. The most effective modifications for improving source control performance were double masking and using a mask brace. Placing a cloth mask over a medical mask blocked ≥85% of cough aerosols and ≥91% of exhaled aerosols. Placing a brace over a medical mask blocked ≥95% of cough aerosols and ≥99% of exhaled aerosols.”
I avoid all indoor meetings and gatherings; I have paused all my photography and interview projects that involve being indoors with another person. Zoom and email is my social life for now.
Isolation is for people who have tested positive for COVID-19. Quarantine is for people who have been exposed to someone with COVID-19. I use “seclusion” to refer to staying apart from others for either reason.
If I am exposed or tested positive with COVID and have to be in quarantine or to isolate, I would only go out into the world again if I get a series of rapid tests that are negative. And I would continue to use masking in indoor spaces shared by others. I would isolate for 10 days if I can’t do a rapid test. PCR tests may be positive long even after you are no longer able to infect others.
Please see our earlier reports for options
We and Our Leaders Can Control COVID
Doom or hope?
Governor Baker, Here's How to Mitigate & Prevent COVID in Housing
Are We Safe Now?
Testimony to Joint Committee on Covid-19
A new peer-reviewed study confirms that COVID is an airborne disease, and reports on the risk of airborne transmission of COVID among persons in a room and creates a model that explains known outbreaks combining masking, ventilation and aerosol-removal rates, number of occupants, and duration of exposure.
Mitigation is greatest with the use of N95 masks, followed by better ventilation and air filtration, and by reducing the time spent in the situation. Other examples of disease transmission include air flowing under doors or through building ventilation systems. The authors apply their model to compare the risk in various situations and methods of mitigation. This information can be used on a community basis to better control the COVID pandemic, and offers some guidance for individual mitigation methods.
"Our analysis shows that mitigation measures to limit shared-room airborne transmission are needed in most indoor spaces whenever COVID-19 is spreading in a community. Among effective measures are reducing vocalization, avoiding intense physical activities, shortening the duration of occupancy, reducing the number of occupants, wearing high-quality well-fitting masks, increasing ventilation, improving ventilation effectiveness, and applying additional virus removal measures (such as HEPA filtration and UVGI disinfection). The use of multiple “layers of protection” is needed in many situations, while a single measure (e.g., masking) may not be able to reduce risk to low levels. We have shown that combinations of some or all of these measures are able to .... [lower the risk and help avoid major outbreaks.]"
Z. Peng et al, Practical Indicators for Risk of Airborne Transmission in Shared Indoor Environments and Their Application to COVID-19 Outbreaks, Environ. Sci. Technol. January 5, 2022 https://doi.org/10.1021/acs.est.1c06531
*Amazing* detailed data on 3rd shots and vaccines from Alberta. Essentially: “The hospitalization rate among 3x-vaccinated 80+ year olds is lower than the hospitalization rate among unvaccinated 12-29-year-olds.”
twitter January 15, 2022
The slow and haphazard acceptance of the evidence of airborne transmission of SARS-CoV-2 by major public health organizations contributed to a suboptimal control of the pandemic; whereas the benefits of protection measures against aerosol transmission are becoming well established (17–20). Quicker acceptance of this evidence would have encouraged guidelines that distinguished rules for indoors and outdoors, greater focus on outdoor activities, earlier recommendation for masks, as well as rules for mask wearing indoors even when social distancing could be maintained, ventilation, and filtration. Earlier acceptance would have avoided the excessive time and money spent on measures like surface disinfection and plexiglass barriers, which are ineffective for airborne transmission and, in the case of the latter, may even be counterproductive (21). https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3904176
Dr. Makoto Tsubokura of the RIKEN Center for Computational Science (R-CCS) talks about his work using the supercomputer Fugaku to do graphic simulations of the spread of COVID-19 through droplets in the air in a variety of situations, such as public transportation and theaters.
Puff the Magic Hater Source: twitter @MsKellyMHayes
They aren't saying: Spread is inevitable, so we need to protect the vulnerable, make healthcare and testing free, and make long term plans to address waves of long COVID.
They're saying: Spread is inevitable, so get back to work and be glad that it's mostly disabled people dying.
Massachusetts Department of Public Health, COVID-19 Dashboard, Weekly Data by City and Town This is the source for positivity data cited in this paper. Follow these steps:
- City & Town Data
- Data by City & Town
- Select County to see city/town
- Select indicator (14-day positivity)
- Scroll to see each city/town
I write based on available evidence and statements by epidemiologists and researchers, even when that evidence is not conclusive or has not been peer-reviewed. I have read a lot of experts' research, but I am not an expert on this topic. I do ask experts to review these writings. This writing is not medical advice. Keep your doctor informed on your symptoms and status.
@coordinatingnow
Citation for this article: Halberstadt, Jerry, The New "How to Avoid COVID," http://stopbullyingcoalition.org/newcovid January 6, 2022, updated & revised on (date) Revised February 10, 2022
